PATHOGENESIS
Shoulder motion is achieved by a combination of glenohumeral joint movement and multidimensional scapular movement. The strong ligaments of the joint capsule and the muscles of the rotator cuff (RC) stabilize the glenohumeral joint. By exerting cranial tensile forces, the shoulder girdle muscles secure the humeral head in its position in the shoulder blade socket.
PATHOGENESIS
Shoulder motion is achieved by a combination of glenohumeral joint movement and multidimensional scapular movement. The strong ligaments of the joint capsule and the muscles of the rotator cuff (RC) stabilize the glenohumeral joint. By exerting cranial tensile forces, the shoulder girdle muscles secure the humeral head in its position in the shoulder blade socket. The scapula is attached to the thorax by muscles. Here, the adhesive suction forces between the fascial layers of the subscapular muscle and the serratus anterior muscle play a crucial role.
The latissimus dorsi and biceps brachii muscles act as antagonists to the shoulder girdle muscles. The humeral head remains in its socket when the tensile forces in the cranial and caudal direction are balanced. If there is no such equilibrium, enthesopathies and myofascial trigger points will develop in the shoulder girdle region.117
If the muscle force caudalizing the humeral head decreases, the humeral head is slightly displaced in the cranial direction and may be decentralized over time. As a result, the rotator cuff, specifically the supraspinal portion of the tendon, is subjected to increased tensile stress. The long lever arm effect of the supraspinatus tendon and the resulting biomechanical benefits achieved when the humeral head is in normal position are gradually lost. Increasing upward displacement of the humerus narrows the subacromial space and so compresses the rotator cuff and subacromial bursa. Weakening of the dorsal scapular muscles due to age or poor posture exacerbates the constriction of the subacromial space. This may be accompanied by more frequent bouts of acute subacromial bursitis.
The constriction results in reduced microcirculation in the insertional region of the rotator cuff, which leads to the degeneration of the supraspinatus tendon. Lowgrade inflammatory processes, continuous bombardment by inflammatory messenger substances and the formation of oxygen radicals attack the tenocytes, causing them to degenerate.119 Intratendinous deposition of calcium apatite crystals represents a further complication affecting the rotator cuff tendons.
The clinical symptoms are those of subacromial pain syndrome. In the medium and long term, destructive structural changes in the subacromial space and osteoarthritic alterations of the acromioclavicular joint (AC joint) occur. Movements in the horizontal plane cause impingement. In many cases, fissures and progressive tendon thinning in the region of the hypovascular insertion of the supraspinatus tendon may occur in the long term, ultimately resulting in tendon rupture (continuum).
HISTORY AND DIAGNOSIS
The incidence of shoulder impingement syndrome increases with age in people over 30 years old. Answers to questions related to jobspecific movements or physical exercise, pain at rest or during activity, sleep disturbed by pain or aching at night, tenderness, pain on exertion, and to acute or chronic symptoms provide valuable information for diagnosis.
During physical examination, the deltoid muscle, scapula position, shape of the spinal column and the AC joint should be checked. Functional tests of the range of motion and specific rotator cuff tests complete diagnostic procedures for shoulder impingement. Examination, palpation and functional tests of the shoulder girdle muscles and their tendon attachments (humerothoracic, scapulothoracic, scapulohumeral muscles) may reveal trigger points which can be identified and instantly treated by means of pressure waves or shock waves.
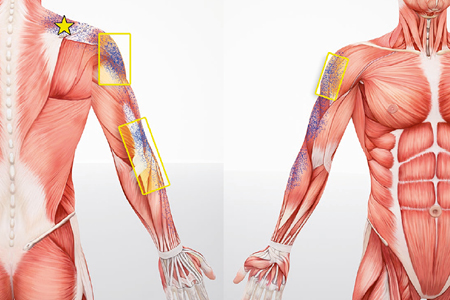
Extracorporeal shock waves (ESW) may induce typical referred pain as illustra- ted below for the supraspinatus and infraspinatus muscles (examples).
Diagnostic Imaging
-
| X-ray, including scapular Y-view, osseous pathologies
-
| Sonography, functional examination, plus PDI (if required)
-
| MRI of pathological morphologies
- Exclusion criteria
-
| Functional or secondary impingement
-
| Vertebrogenic, vascular or neurovascular causes
-
| Entrapment neuropathy of the spinal accessory nerve at the point where it emerges dorsally from the sternocleidomastoid (SCM) muscle or where it enters the trapezius muscle; adhesions after ENT surgery (e.g. neck dis- section)
-
| Traction/compression of the suprascapular nerve in the suprascapu- lar notch, especially after RC rupture caused by medial displacement of muscles120, 121
-
| Compression of the axillary nerve between the head of triceps and teres major muscles in the lateral axillary foramen (overhead work)120
-
| Neuralgic shoulder amyotrophy
-
| Complete rotator cuff rupture
-
| Acute subacromial bursitis with reactive effusion in the synovial sheath of
the long biceps tendon
Weitere Informationen zu diesem Artikel finden Sie in unserem Fachbuch von Ulrich Dreisilker.
Mit einem Klick zu unseren informativen Fachbüchern im Bereich Stoßwellen-Therapie.
Informieren Sie sich jetzt!
Jetzt informieren: Level-books.com
